‘We didn’t know if our boys would survive’
After family endures childhood cancer, a traumatic car crash threatens two sons’ lives.
Article Author: Vikki Mioduszewski
Article Date:
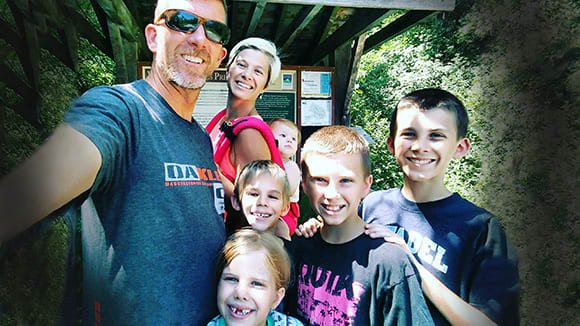
July 25, 2018, wasn’t the first time Orange Park’s Hale family faced their worst nightmare, even though Karina and Kurt Hale had just learned that two of their five children, Seth and Jaden, had been in a horrible car crash and their survival was far from assured.
Just four-and-a-half years ago, when Seth was 7, he was diagnosed with cancer at Wolfson Children’s Hospital after a visit to the Wolfson Children’s Emergency Center at Baptist Clay. Pediatric emergency medicine physician Matthew Locklair, MD, with Emergency Resource Group (ERG) transferred Seth directly to the hematology/oncology unit at Wolfson Children's, where testing revealed the diagnosis of acute lymphoblastic leukemia (ALL), which commonly has a survival rate of up to 90 percent with chemotherapy treatment.
Nemours Children’s Health pediatric hematologist/oncologist Manisha Bansal, MD, ordered genetic testing in order to customize Seth’s treatment and to rule out any other conditions that could affect his outcome.
To the Hales’ dismay, genetic testing showed Seth’s leukemia cells were hypodiploid, a chromosomal condition that only worsened his ALL prognosis and dropped his survival rate down to 40 percent with standard chemotherapy. “Dr. Bansal held my hand and cried with me when she told me,” Karina said.
Chemotherapy and radiation treatment would not be enough to give him the best chance at a cure. “The oncology team had already studied to know the best chance Seth had to beat his cancer was a bone marrow transplant at Wolfson Children’s, so we changed gears from just chemo to pursue a transplant,” said Karina.
Their next challenge was finding a bone marrow donor who matched Seth. The odds of finding a marrow donor match within the family – what Seth would need to have the best chance at survival – were low. Each of their children had only a 25 percent chance of being a match for their brother. Still, the whole family – Karina and Kurt, older brother Jaden and the Hales’ three-year-old twins, Erik and Lydia – were tested.
To their amazement, the twins – despite being fraternal rather than identical – proved to both be 100-percent matches for Seth.
‘So much life in him, he had some to share’
Karina and Kurt had a dilemma. Which of their twins would they choose to be Seth’s donor, which would involve anesthesia and an extraction procedure in the OR, not without risk?
“Turns out, it was easy,” Karina said. “We felt like Erik was so full of life, stronger and bigger than his sister. And he had so much life to share.”
Erik had his bone marrow extraction on July 29, 2014. Kurt said, “Within hours of his procedure, Erik was playing basketball in his room. He didn’t even have Tylenol. He bounced right back.”
Erik’s bone marrow was healthy and plentiful and was transfused into Seth the same day.
Only three weeks later, Seth was back home, where he faced 100 days of isolation to protect him from infection while his immune system returned. After that, life returned to normal for the Hale family, with Karina homeschooling their four kids, Kurt running the family business, and the whole family busy at their church, Hibernia Baptist.
Family beach day turns into a struggle for survival
“My sister was visiting from Michigan, and we’re beach bums, so we decided to have a beach day in St. Augustine,” said Karina, recalling that sunny day. “Jaden had a tummy ache and wanted to stay home, but I didn’t want to leave him alone, so I told him we would get him something to settle his stomach and we would just lie on the beach.”
Karina’s father Daniel King took the older boys, Jaden and Seth, in his car, while Karina and her sister took the little ones in a separate vehicle.
Karina remembered: “We were 10 minutes ahead of them, and had just crossed over the Shands Bridge in Green Cove Springs when I got a call from Dad. He said, ‘We’ve been in an accident.’ I asked him how the boys were, and he said, ‘I don’t know,' because he was in shock or had a concussion.”
Traffic was backed up so Karina got out of her car and ran toward the crash scene at the intersection of US 17 and 16. “I saw the second ambulance pull away and I couldn’t get in there with them,” she said. “They were already on their way to the [Pediatric] Trauma Center at Wolfson Children’s Hospital.”
Karina was horrified by what she saw at the collision scene. A semi-truck had plowed into the passenger side of her father’s car. It seemed hard to imagine how anyone could survive such a terrible crash. She had little time to process that, though, and got in her car to pick Kurt up and head to the hospital.
Kurt said, “We had no idea how the boys were. Were they just shaken up? Were they OK or not OK? Waiting for Karina to pick me up seemed like forever, even though it was actually about 25-30 minutes with traffic. I saw the ambulances carrying our sons go by while I was waiting for her.”
The Hales prayed. “I told God, ‘I know you gave me these boys and that you love them even more than I do,’" said Karina. "I prayed that we would get to keep both of them, but knew that if this was their last day, they would be with Him. That’s the way I got through that drive.”
True extent of injuries discovered at Wolfson Children’s Pediatric Trauma Center
When Karina and Kurt arrived at the hospital, they went to the Trauma Center, where Jaden and Seth had adjoining rooms so pediatric emergency medicine doctors Suman Mayer, MD, and Brian Gilligan, MD, both with ERG, plus the rest of the trauma team, could work on both critically injured boys.
Kurt said, “There was blood everywhere. Seth looked visibly worse, but Jaden actually turned out to be more critical due to internal injuries. Jaden started seizing and they told us they had to get a CT scan right away.”
The scan showed that Jaden’s skull was fractured in the front, over the right eye, and it had punctured his brain, leading to a bruise and the brain and internal bleeding. Pediatric neurosurgeon Nathan Ranalli, MD, and craniofacial surgeon Barry Steinberg, MD, both with the UF College of Medicine – Jacksonville, were called in.
“After his seizure, Jaden’s mental status deteriorated and he had to be intubated,” Dr. Ranalli said. “Given the head CT finding of a depressed skull fracture causing compression of his brain, emergency surgery was indicated to relieve the pressure and repair the defect.”
“The nature and severity of Jaden’s injuries required we remove the back wall of his frontal sinus (next to his brain) and close its communication with his nose; these are usually connected by an opening between the two but in Jaden’s case, it was closed off,” explained Dr. Steinberg. “After that, we reconstructed his forehead using his fractured bone and titanium metal mesh.”
Thankfully, the procedure went well and Jaden’s intracranial pressure returned to normal. However, Jaden’s ordeal wasn’t over. At the end of brain surgery, Nemours pediatric anesthesiologist Fernandez Zayas-Bazan, MD, noted that Jaden’s blood pressure had dropped dramatically, leading physicians to suspect Jaden had an abdominal injury that wasn’t visible when he first arrived at the Trauma Center.
After an ultrasound showed blood in Jaden's abdomen, Nemours pediatric trauma surgeon Nicholas Poulos, MD, performed exploratory surgery. “Jaden’s muscle layers in his stomach had separated in the accident, causing a small blood vessel to very slowly leak blood into his abdomen,” explained Dr. Poulos. “I had to perform a stomach degloving procedure, in which I reattached the muscle layers, and stopped the bleeding by cauterizing the blood vessel.”
Back on the Pediatric Intensive Care Unit (PICU), the Hales waited anxiously for news of Jaden while caregivers cleaned glass out of Seth’s face. “He got 18 stitches on his forehead, inside his nose, and on his chin,” said Kurt. “He also had a bruise and bleeding on his brain but didn’t require surgery. We sat with him for hours and hours while Jaden was being treated in the OR.”
Following Jaden’s surgery, Dr. Poulos came to talk to the Hales. “He said he could tell us what happened, but that would be a lot of medical terms, so it would be better for him to show us,” said Kurt. “It was good he did that because we could see exactly what we were dealing with because he walked us through it.”
While Seth was doing OK, Jaden was still in critical condition. Kurt and Karina relied on their faith. “It can be easy to have faith when your kids are healthy and life is good,” Kurt said. “When you’re faced with losing the dearest things to you, you learn the depth of your faith and the strength God gives.”
While Seth went home from the hospital only four days after the accident, Jaden remained sedated, on a ventilator and with a feeding tube in the PICU. Night three into his hospital stay, he had improved enough to be taken off the ventilator.
While he has a long road to recovery ahead, Jaden was well enough to be transferred to a regular floor at Wolfson Children’s on July 30.
“The first thing he said when he woke up was, ‘Daddy, you have the weirdest smile,’” said Kurt. “We knew our quick, witty and smart Jaden was back.”
Home to hospital to home again
Jaden was discharged from Wolfson Children's on August 12 – huge progress considering his condition just a couple of weeks before.
“Seth is completely better, his stitches are already out and he looks amazing!” said Karina.
Now a family of seven after the birth of baby girl Norah last year, the Hales are grateful for the way the Wolfson Children’s Hospital team has surrounded them with care for the last few years. “This hospital is like our family,” said Karina. “We wouldn’t take our kids anywhere else.”
Dr. Poulos, who serves as medical director of Wolfson Children’s Pediatric Trauma Center, said: “Jaden has a long road ahead of him as he recovers from his injuries, but he is healing well. It is so important for a child to have a lot of support, and Jaden is lucky to have such a big, caring family in his corner. Having a Pediatric Trauma Center that brings together all of these medical and surgical specialties, in one location, is also critically important when minutes matter and when a delay in care can change a child's life."