C-shaped sickness
Sickle cell complications may vary from mild to severe.
Article Author: Johnny Woodhouse
Article Date:
Even though it was first identified in the U.S. as early as 1910, sickle cell disease (SCD), a group of inherited red blood cell disorders that primarily affect people with African heritage, wasn’t widely known until the 1970s.
Today, it is considered the most common inherited blood disorder in the world and a major public health concern.
SCD may result in chronic pain episodes, severe infection, organ damage, stroke and acute chest syndrome, which includes chest pain, cough, fever, and low oxygen levels,” said Cynthia Gauger, MD, a pediatric hematologist/oncologist with Nemours Children’s Health, Jacksonville who treats SCD patients at Wolfson Children’s Hospital.
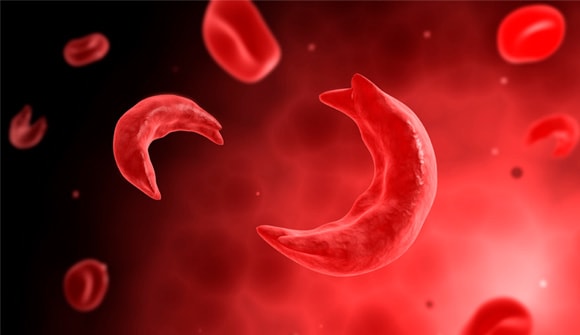
SCD begins when healthy red blood cells lose their flexible shape and become hard and sticky, clogging blood flow, Dr. Gauger said.
The infected cells take on the shape of a sickle, a farming tool with a semicircular or C-shaped blade. The normal lifespan of healthy red cells is between 90 and 120 days. SCD red cells die early, basically every 10 to 20 days, causing a constant shortage.
According to the Centers for Disease Control and Prevention (CDC), SCD affects approximately 100,000 Americans each year. It occurs in one out of every 365 African-American births and one of out of every 16,500 Hispanic-American births.
Sickle cell trait
One out of every 13 African Americans are born with the sickle cell trait and may pass it on to their children. Sickle cell trait happens when a person inherits one sickle cell gene and one normal gene.
The most severe form of SCD is sickle cell anemia, where a person inherits one sickle cell gene from each parent. Other often milder forms of SCD occur when a person inherits one sickle cell gene and another abnormal hemoglobin gene.
Diagnosis and treatment
SCD is diagnosed through newborn screening at birth. Children may show signs of the disease in the first year of life.
“Newborn screens have really helped us identify these children at birth so we can treat them as soon as possible,” said Dr. Gauger, a physician for more than 30 years. “And very exciting research in therapy is now ongoing.”
In the past three years, four new drugs have been approved to treat SCD, and two new drugs are currently in Phase II trials, according to the Federal Drug Administration.
Because each SCD case is clinically different and complications may vary from mild to severe, the mainstay treatment is hydroxyurea, a drug that helps prevent the formation of sickle-shaped red blood cells.
“Hydroxyurea is the single-best treatment we have right now, and studies show it’s safe to administer as early as nine months of age,” Dr. Gauger said. “We use it to prevent complications, not treat complications.”
If a suitable donor can be found, SCD may be cured through a bone marrow transplant.
Genetic counseling can help
Before trying to conceive, people who carry the sickle cell trait should make an appointment with a genetic counselor so they can understand their risk of having a child with sickle cell anemia. Counselors can also explain possible treatments, preventive measures and reproductive options.
“Genetic counseling is important and I wish pediatricians discussed it even more with parents of children with SCD,” added Dr. Gauger.
“We follow more than 250 patients each year with some form of SCD, but fortunately only a small number of these individuals need to be hospitalized, which we are very thankful for.”
One way to help fight SCD is to donate blood, which helps ensure that SCD patients get blood which is most compatible with their blood type and subtype. To donate, visit LifeSouth.
Pediatric health care partners Wolfson Children’s Hospital and Nemours Children’s Health, Jacksonville, offer complete care for children with sickle cell disease. For more information on SCD, talk to your child’s pediatrician. To schedule an appointment with a pediatric hematologist/oncologist, call 904.697.3600.



